CTAK Reimbursement
CorneaGen offers free CTAK reimbursement and medical claims assistance to help guide you in billing to your local Medicare carrier and other commercial insurance carriers. Our internal resources in conjunction with 3rd party health care consultants, will help with coding, coverage, and reimbursement inquiries.
Procedure Overview
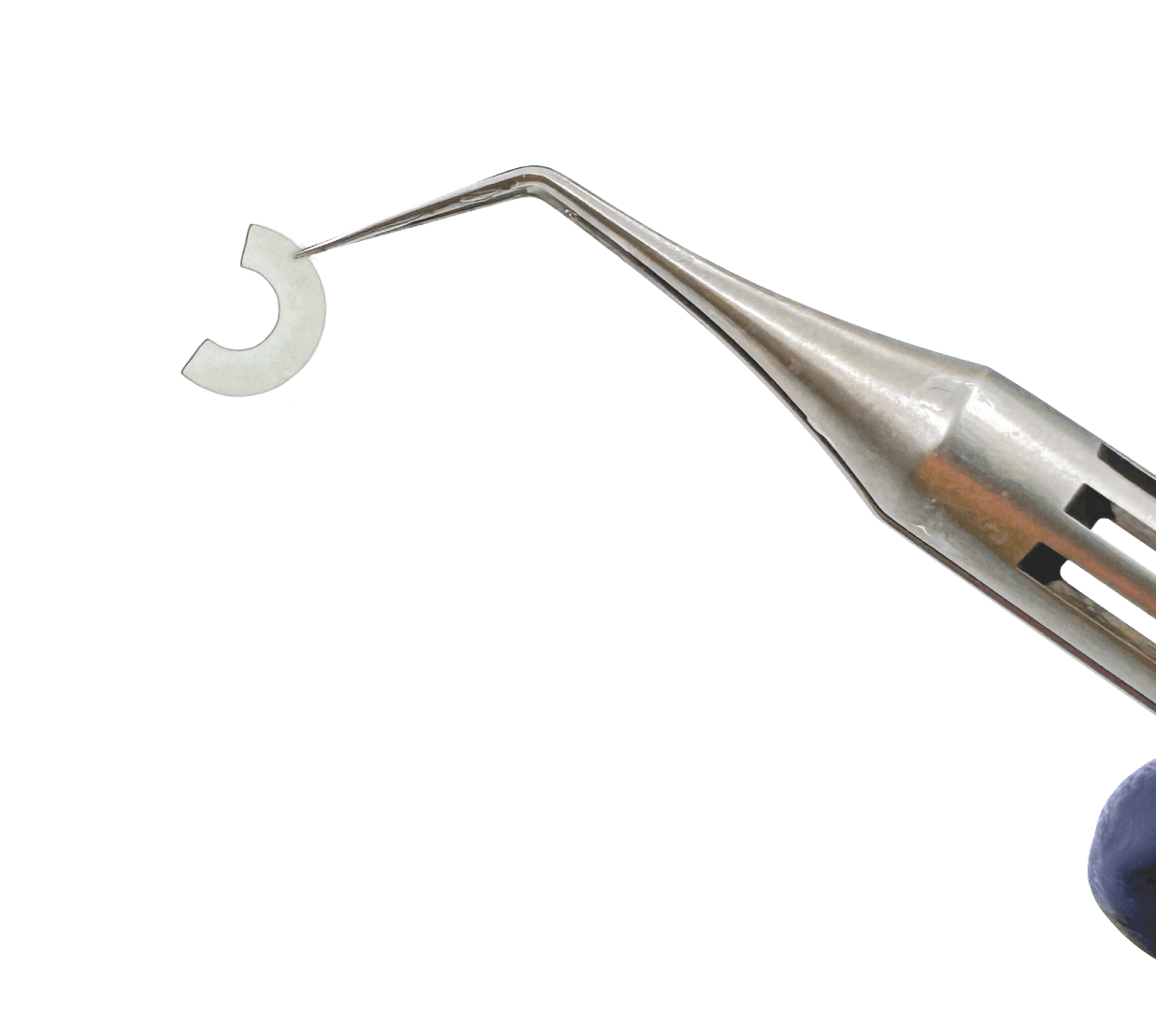
Corneal Tissue Addition Keratoplasty (CTAK) is the latest advancement in keratoconus treatment, offering enhanced accuracy and precision for both patients and surgeons. This innovative procedure utilizes a CTAK inlay designed to optimize corneal flattening, improve visual acuity, and increase corneal thickness. Unlike full-thickness corneal transplantation, CTAK preserves native corneal tissue by implanting a customized, gamma-irradiated corneal inlay into a laser-created corneal pocket.
This web guide provides a detailed breakdown of billing, reimbursement, and common payer considerations for CTAK, including procedure, tissue acquisition, laser usage, and facility-specific billing nuances.
Looking for reimbursement resources for a different tissue type?
We also offer comprehensive reimbursement resources for: Corneal Tissue, VisionGraft, and BrightMEM.
CTAK Reimbursement
Primary Procedure & Tissue Codes
When the laser channel creation (i.e. stromal bed preparation) and anterior lamellar graft implantation occur on the same day, the procedure may be billed using the codes below.
| Code | Description |
|---|---|
| CCPT® 65710 | Anterior Lamellar Keratoplasty surgical procedure |
| HCPCS V2785 | Processing, preserving, and transporting corneal tissue |
Modifiers to Consider
| Modifier | Description | Usage |
|---|---|---|
| LT or RT | Left Side OR Right Side Procedure | Modifier(s) used for determination of which eye is receiving the procedure |
| -22 | Increased Procedural Services |
Used when work required for the procedure is substantially greater than typically required. This can be related to procedural or time-added complexities |
| -23 | Non-Standard Anesthesia | Modifier used when anesthesia is used outside of the standard local anesthesia practices for corneal transplant |
| -24 | Patient Evaluation for Unrelated Procedure |
Used when a physician or other qualified healthcare professional provides evaluation services unrelated to the procedure during post-op period |
| -50 | Bilateral Procedure | Used when the procedure occurs for both eyes in the same surgical session |
| -51 | Multiple Procedures | Used when multiple procedures other than anterior lamellar keratoplasty are performed in the same surgical session |
| -59 | Distinct Procedural Service |
Used when indicating a procedure or service was performed that is independent of other services on the same day separate from the procedure |
| -76 | Repeat Procedure, Same Physician |
Used when the procedure needs to be repeated by the same physician |
| -78 | Unplanned Return to Procedure Room |
Used in circumstances where the patient has returned to the OR for procedures related to the initial procedure during the recovery period |
| -79 | Unrelated Procedure by Same Physician Post-Op |
Used in circumstances where an unrelated procedure is performed during the post-operative period |
Medicare Reimbursement for CTAK
Coverage Considerations
CTAK is eligible for Medicare reimbursement when deemed medically necessary.
Separate reimbursement for corneal tissue (V2785) is allowed based on the actual cost from the eye bank, which must be supported by an invoice.
When CPT 65710 is used, Prior Authorization is generally not required for Medicare, but proper documentation of medical necessity is essential.
Medicare Payment by Facility Type
| Setting | Billing Considerations | Reimbursement Details |
|---|---|---|
| Hospital Outpatient (HOPD) | Billed under Ambulatory Payment Classification (APC) |
Medicare reimburses separately for corneal tissue (HCPCS code V2785). Medicare Status Indicator “F” ensures corneal tissue is paid at reasonable cost outside the Outpatient Prospective Payment System (OPPS) |
| Ambulatory Surgery Center (ASC) |
CPT® 65710 reimbursed under ASC payment system |
V2785 is separately payable, CTAK is eligible for Medicare reimbursement when deemed medically necessary. Separate reimbursement for corneal tissue (V2785) is allowed based on the actual cost from the eye bank, which must be supported by an invoice. When CPT 65710 is used, Prior Authorization is generally not required for Medicare, but proper documentation of medical necessity is essential. |
| Physician’s Office | Medicare generally does not reimburse facility fees |
Requires payer-specific approval. |
Required Documentation for Medicare
- Surgeon’s operative report
- Eye bank invoice (for V2785 reimbursement)
- Medical necessity justification (keratoconus diagnosis, previous failed treatments, etc.)
CorneaGen has an extensive library of pre-authorization and appeal documents available for use to assist you with your insurance payer discussions. You can access those letters at below in the Additional Resources or reach out to your Surgical Product Specialist for additional information
Commercial Payer Reimbursement for CTAK
Coverage Considerations
- Coverage varies widely by insurer. Some commercial plans consider CTAK investigational, making prior authorization critical.
- Some payers bundle corneal tissue costs into procedural payments, meaning HCPCS V2785 may not be separately reimbursed.
Medicare Payment by Facility Type
| Setting | Billing Considerations | Reimbursement Details |
|---|---|---|
| Hospital Outpatient (HOPD) | CPT® 65710 and HCPCS V2785 billed separately |
Some plans bundle corneal tissue into procedural payment. |
| Ambulatory Surgery Center (ASC) |
ASC facility fee may be reimbursed separately | Prior authorization required for both procedure and tissue. |
| Physician’s Office | If approved, procedure fee may be covered | Facility fee is not covered, limiting financial viability in-office |
Required Documentation for Commercial Payers
- Prior authorization confirmation
- Medical necessity justification
- Invoice for corneal tissue (if V2785 is separately reimbursed)
Exceptions
Some regional commercial insurance providers outsource bill processing of corneal tissue to a third-party health plan administrator. Those administrators may require different coding than V2785. A list of commercial insurance companies known to use a third-party administrator is below. For those listed in the regions below, it is encouraged to review your insurance contract for billing procedures or contact CorneaGen at Contracts@CorneaGen.com so we can help you connect with the appropriate personnel at the Administrator’s office.
- Aetna – Nationwide
- Anthem – CA, NV, GA, OH, NH, CT, IN
- BCBS – FL, NC
- CBC – PA
Key Considerations
- Verify insurance coverage and benefits prior to performing CTAK.
- Submit corneal tissue invoices (Medicare and nearly all commercial payers require this).
- Be prepared to negotiate reimbursement rates with commercial payers.
- Understand prior authorization processes and documentation requirements for both Medicare and commercial payers.
- Include the eye bank invoice with any payment request submissions to your insurance payer.
- For CPT 65710, applicable modifiers must be used correctly to avoid claim denials.
- Describe the procedure as “Anterior Lamellar Keratoplasty” in all payer communications. Terminology such as refractive or astigmatism correction should be avoided in the reimbursement request as these may suggest elective procedures and jeopardize medical necessity-based coverage.
We Offer Reimbursement Consultation Services
If you need assistance with reimbursement of corneal tissue, CorneaGen is pleased to provide its customers with reimbursement and medical claims assistance to help guide you in billing corneal tissue to your local Medicare carrier and other commercial insurance carriers.
You can receive reimbursement consultation services free of charge, through NMD HealthCare consulting. NMD is fully prepared to receive and respond to all of CorneaGen’s customers’ coding, coverage and reimbursement inquires.
Please reach out to your CorneaGen Surgical Product specialist so that they can connect you with a NMD representative. For more information on NMD, visit their website.
Frequently Asked Questions
In most cases, no. There is currently no specific CPT® or HCPCS code that supports separate reimbursement for laser use when it is part of a covered procedure such as CPT 65710 (Anterior Lamellar Keratoplasty). Key guidance includes:
- Separate billing for laser usage is typically not allowed under Medicare or most commercial payer policies.
- Assignment of Benefits Considerations: Charging the patient directly for laser use as an out-of-pocket “click fee” during a covered service may violate payer assignment rules and expose the facility or surgeon to compliance risk or audit.
- Payer Variability: Some commercial payers may allow billing for laser use if specifically justified with medical necessity documentation and payer authorization. These cases are contract specific.
While the preferred approach—aligned with AAO guidance—is to perform both steps on the same day to support clean reimbursement under CPT 65710 (Anterior Lamellar Keratoplasty), we recognize that in some clinical settings, staging may be unavoidable.
In such cases:
- Procedure Coding: Facilities may consider billing the procedure under CPT 66999 (Unlisted procedure, anterior segment of eye) when staging is unavoidable. However, this approach may result in reduced or uncertain reimbursement, typically requires extensive documentation, and may trigger payer review or processing delays. We recommend obtaining prior authorization and confirming payer-specific guidance before proceeding with this approach.
- Tissue Coding: Regardless of the surgical timing, the donor tissue component should still be reported separately under HCPCS V2785 (Processing, preserving, and transporting corneal tissue).
- Audit & Compliance Risks: Performing procedures in different facilities or on different days increases the risk of coding discrepancies, especially if payers view CPT 65710 as inclusive of preparatory steps like channel creation. AAO recommends avoiding split billing unless it is unavoidable.
- Best Practice: When feasible, coordinate surgical scheduling to allow same-day channel creation and graft implantation, performed by the same surgeon in a single operative session. This ensures alignment with payer policy and maximizes the likelihood of appropriate reimbursement.
When billing CPT 66999 (Unlisted procedure, anterior segment of eye)—such as when the laser channel creation and graft implantation are performed on different days or in different facilities:
- For public payers, an Advance Beneficiary Notice (ABN) should be signed by Medicare patients to acknowledge potential non-coverage. In addition, Box 19 of the CMS-1500 claim form should include a brief description of the procedure to assist with payer review.
- For commercial payers, providing a fee schedule for similar ALK procedures (such as CPT 65710) may help inform reimbursement rates when submitting CPT 66999
- Use applicable modifiers when billing CPT 66999 to avoid claim denials